Fill Your Annual Physical Examination Form
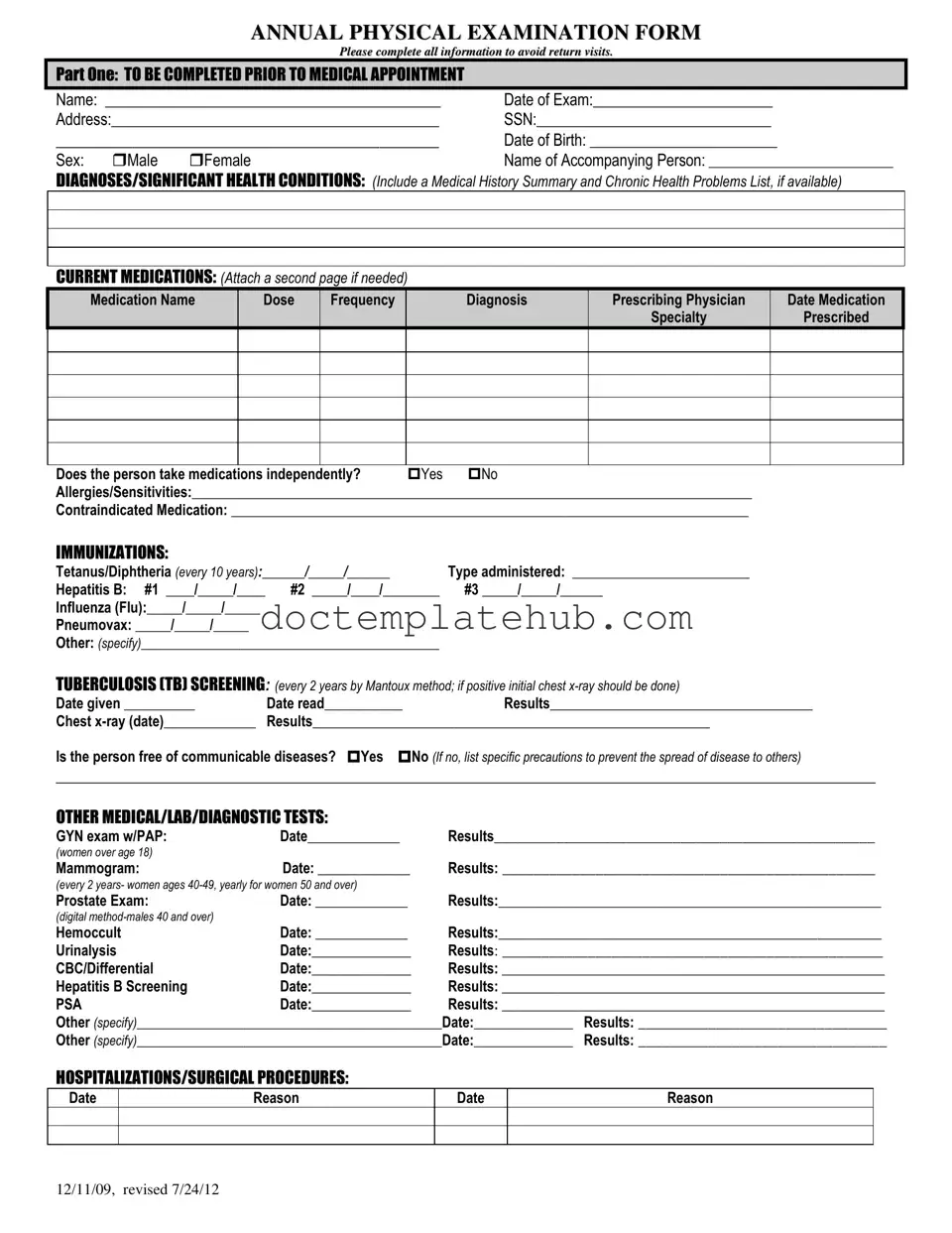
The Annual Physical Examination form serves as a comprehensive tool designed to gather essential health information from patients prior to their medical appointments. This form is divided into two main parts, each aimed at ensuring that healthcare providers have a complete understanding of a patient's medical history and current health status. In the first section, patients are required to provide personal details such as their name, date of birth, and contact information, alongside critical health information, including any existing diagnoses, current medications, allergies, and vaccination history. This information is vital for healthcare providers to tailor their examinations and treatments effectively. The second part of the form focuses on the general physical examination, where healthcare professionals document vital signs like blood pressure and pulse, as well as evaluate various bodily systems for normal findings. Additional sections allow for comments on any necessary follow-ups, recommendations for health maintenance, and details regarding any special considerations or limitations that may affect the patient’s daily activities. By meticulously completing this form, patients can help facilitate a thorough and efficient examination, ultimately contributing to better health outcomes.
Similar forms
The Annual Physical Examination form shares similarities with a Medical History Questionnaire. Both documents require individuals to provide comprehensive information about their health history, including past medical conditions, surgeries, and current medications. This information is crucial for healthcare providers to assess a patient’s overall health and to identify any potential risks. Just as the Annual Physical Examination form prompts for details on chronic health problems, the Medical History Questionnaire typically includes sections for allergies and previous illnesses, ensuring that the physician has a complete understanding of the patient's medical background.
Another document akin to the Annual Physical Examination form is the Immunization Record. Both forms emphasize the importance of vaccination history, ensuring that individuals are up-to-date with necessary immunizations. The Annual Physical Examination form outlines specific vaccines and their administration dates, similar to how an Immunization Record tracks each vaccine received over time. This shared focus on immunization helps healthcare providers determine the need for any additional vaccinations and assess the patient's overall immunity status.
In the realm of business, protecting confidential information is paramount, and a New York Non-disclosure Agreement serves as a vital tool in this regard. Beyond the essentials of safeguarding trade secrets, it establishes trust between parties and maintains the integrity of sensitive data throughout negotiations. For those looking to draft or understand such agreements, resources like smarttemplates.net can provide valuable templates and guidance, ensuring that all necessary legal protections are effectively addressed.
A Health Risk Assessment (HRA) is also comparable to the Annual Physical Examination form. Both documents aim to evaluate an individual's health risks and lifestyle choices. The HRA often includes questions about diet, exercise, and tobacco use, paralleling the recommendations for health maintenance found in the Annual Physical Examination form. By identifying risk factors, both documents assist healthcare providers in creating tailored health plans to improve patient outcomes.
Lastly, the Consent for Treatment form bears similarities to the Annual Physical Examination form in that both require patient acknowledgment and understanding of the medical procedures involved. While the Annual Physical Examination form focuses on gathering health information, the Consent for Treatment form ensures that patients are informed about the examinations and treatments they will undergo. This mutual emphasis on patient awareness promotes transparency and trust between healthcare providers and patients, ultimately enhancing the quality of care received.
Other PDF Templates
Ssa 44 Instructions - Detailed income reporting through the SSA-44 can foster better support from Social Security.
Obtaining the CDC U.S. Standard Certificate of Live Birth is essential for new parents, as it provides a legal record of their child's birth and is necessary for various processes, including applying for a Social Security number. For those interested in understanding or accessing this vital document, further information can be found at https://documentonline.org/blank-cdc-u-s-standard-certificate-of-live-birth/.
How to Ship Freight - The form states it is not negotiable and refers to specific rules of service.
Free Direct Deposit Form Pdf - Submissions of this form are generally straightforward and easy to follow.
More About Annual Physical Examination
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to gather essential health information prior to a medical appointment. This information helps healthcare providers assess a patient's overall health, identify any significant health conditions, and recommend appropriate care or follow-up actions. Completing the form accurately ensures that patients receive the best possible care without the need for return visits due to missing information.
What information is required in Part One of the form?
Part One requires personal details such as the patient's name, date of birth, address, and social security number. Additionally, patients must list any significant health conditions, current medications, allergies, and immunization history. This section helps the healthcare provider understand the patient's medical background and current health status.
How should current medications be documented?
Patients should list each medication, including the name, dosage, frequency, diagnosis for which it was prescribed, and the prescribing physician. If more space is needed, an additional page can be attached. It is also important to indicate whether the patient takes medications independently.
What immunizations need to be reported on the form?
The form requests information on several immunizations, including Tetanus/Diphtheria, Hepatitis B, Influenza (Flu), and Pneumovax. Patients should provide the dates of administration and specify the type of immunizations received. Keeping this information up to date helps ensure that patients remain protected against preventable diseases.
What is the significance of tuberculosis (TB) screening?
TB screening is crucial for identifying individuals who may have been exposed to tuberculosis. The form specifies that TB screening should be done every two years using the Mantoux method. If the initial screening is positive, a chest x-ray is required to determine if the individual has an active infection.
What should be included in the evaluation of systems section?
This section requires the healthcare provider to evaluate various body systems, including eyes, ears, lungs, and cardiovascular health. Providers will mark whether findings are normal or not and may add comments for any abnormalities. This comprehensive assessment helps in identifying potential health issues that may require further investigation.
How can patients prepare for their physical examination?
Patients should complete the Annual Physical Examination form thoroughly and bring any relevant medical records to their appointment. It is also advisable to compile a list of current medications and any questions or concerns about their health. This preparation helps ensure a productive visit with the healthcare provider.
What happens if the form is not completed correctly?
If the form is not completed correctly, patients may need to schedule additional appointments to provide the missing information. This can lead to delays in receiving care and may require patients to revisit their healthcare provider more frequently than necessary. Accurate and complete information helps streamline the examination process.
Dos and Don'ts
When filling out the Annual Physical Examination form, keep these important tips in mind:
- Be sure to fill in all required fields completely to avoid any delays.
- Double-check your personal information for accuracy, including your name and date of birth.
- List all current medications, including dosage and frequency, even if they seem minor.
- Indicate any allergies or sensitivities clearly to help your healthcare provider.
- Provide a brief medical history summary, including any chronic health problems.
Here are some things you should avoid:
- Do not leave any sections blank; incomplete forms may lead to return visits.
- Avoid using medical jargon or abbreviations that may confuse the reader.
- Do not forget to sign and date the form before submission.
- Refrain from providing outdated or incorrect information regarding past medical conditions.
Annual Physical Examination - Usage Steps
After gathering the necessary information, you will be ready to complete the Annual Physical Examination form. This form requires personal details, medical history, current medications, and various health evaluations. Ensure that all sections are filled out completely to avoid any delays in your appointment.
- Start with PART ONE. Fill in your Name, Date of Exam, and Address.
- Provide your Social Security Number and Date of Birth.
- Indicate your Sex by checking the appropriate box.
- Write the Name of Accompanying Person if applicable.
- List any Diagnoses/Significant Health Conditions you have, including a medical history summary if available.
- Under Current Medications, fill in the details of each medication, including name, dose, frequency, diagnosis, prescribing physician, and date.
- Indicate if you take medications independently by checking 'Yes' or 'No'.
- List any Allergies/Sensitivities and any Contraindicated Medications.
- Fill in your Immunizations details, including dates and types administered.
- Complete the Tuberculosis (TB) Screening section with the date given, date read, and results.
- Provide information on other medical/lab/diagnostic tests, including dates and results.
- List any Hospitalizations/Surgical Procedures with dates and reasons.
- Move to PART TWO. Fill in your Blood Pressure, Pulse, Respirations, Temperature, Height, and Weight.
- For each system in the Evaluation of Systems section, indicate if the findings are normal by checking 'Yes' or 'No'.
- Complete the Vision Screening and Hearing Screening sections, noting if further evaluation is recommended.
- Provide any Additional Comments regarding your medical history, medications, and recommendations for health maintenance.
- Indicate if there are any limitations or restrictions for activities.
- Note if you use adaptive equipment and any changes in health status from the previous year.
- Complete the physician’s information section, including the name, signature, date, address, and phone number.