Fillable Do Not Resuscitate Order Template for Arizona State
The Arizona Do Not Resuscitate (DNR) Order form serves as a crucial document for individuals who wish to communicate their preferences regarding medical interventions in the event of a life-threatening situation. This form is particularly important for those with serious medical conditions or advanced age, as it allows them to express their desire to forgo resuscitation efforts, such as chest compressions or artificial ventilation, should their heart stop or they stop breathing. The DNR Order must be signed by a physician, ensuring that the decision is made with professional guidance. Additionally, it is vital for the individual to discuss their wishes with family members and healthcare providers to ensure everyone understands the implications of the order. The form is designed to be easily accessible, often carried by the individual or placed prominently in their medical records. By understanding the DNR Order, individuals can take proactive steps to align their medical care with their personal values and preferences, fostering a sense of control during challenging times.
Similar forms
The Arizona Do Not Resuscitate (DNR) Order form shares similarities with the advance directive, a broader legal document that outlines an individual’s preferences for medical treatment in the event they become unable to communicate their wishes. Like the DNR, an advance directive allows individuals to specify what types of medical interventions they do or do not want, ensuring that their healthcare aligns with their personal values and desires. Both documents serve to guide healthcare providers and loved ones in making decisions that respect the individual’s choices regarding end-of-life care.
Another document akin to the Arizona DNR is the living will. A living will specifically addresses the types of medical treatments an individual wishes to receive or refuse if they are terminally ill or in a persistent vegetative state. Similar to the DNR, a living will provides clarity to healthcare providers and family members, helping to avoid confusion during critical moments. Both documents emphasize the importance of respecting a person's autonomy and preferences regarding life-sustaining treatments.
The medical power of attorney (POA) is also comparable to the Arizona DNR Order. This document allows an individual to designate someone else to make healthcare decisions on their behalf if they become incapacitated. While the DNR focuses specifically on resuscitation efforts, the POA can cover a wider range of medical decisions, including those related to end-of-life care. Both documents empower individuals to ensure their healthcare preferences are honored, whether directly or through a trusted representative.
Understanding the nuances of a Transfer-on-Death Deed process in Georgia can be crucial for property owners looking to ensure a smooth transition of their assets upon death. This legal instrument simplifies asset distribution and eliminates the need for probate, allowing heirs to inherit property directly and efficiently.
Similar to the DNR, a Physician Orders for Life-Sustaining Treatment (POLST) form serves as a medical order that details a patient’s preferences for life-sustaining treatments. The POLST is often used for individuals with serious health conditions and provides specific instructions that healthcare professionals must follow. Like the DNR, it is designed to communicate a patient’s wishes clearly and effectively, facilitating a shared understanding among healthcare providers, patients, and families.
The do-not-intubate (DNI) order is another document that shares similarities with the Arizona DNR. A DNI specifically instructs healthcare providers not to place a patient on a ventilator if they stop breathing or their breathing becomes inadequate. While the DNR addresses all resuscitation efforts, the DNI focuses solely on the use of intubation and mechanical ventilation. Both orders reflect a patient’s preferences regarding aggressive life-saving measures, ensuring that their wishes are respected in critical situations.
The comfort care order is also comparable to the DNR form. This document emphasizes the importance of providing comfort to patients rather than pursuing aggressive treatments that may prolong suffering. Like the DNR, a comfort care order prioritizes the quality of life for individuals facing terminal conditions. Both documents aim to ensure that patients receive compassionate care aligned with their values and preferences during their final days.
A no-code order is another document that bears resemblance to the Arizona DNR. A no-code order indicates that healthcare providers should not perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. While the DNR covers a broader range of resuscitation efforts, the no-code order specifically focuses on the act of resuscitation itself. Both documents serve to communicate a patient’s wishes regarding emergency interventions, ensuring that their choices are honored in life-threatening situations.
The hospice care plan is also similar to the Arizona DNR in that it focuses on providing comfort and support to individuals facing terminal illnesses. This plan outlines the goals of care, which may include pain management and emotional support, while avoiding aggressive treatments that could prolong life without improving its quality. Both the hospice care plan and the DNR reflect a commitment to honoring a patient’s wishes and ensuring that their final days are spent in dignity and comfort.
Lastly, the treatment limitation order is comparable to the Arizona DNR. This document specifies particular medical interventions that should not be performed, similar to the DNR's focus on resuscitation efforts. Treatment limitation orders can be tailored to individual preferences and may encompass a range of interventions beyond resuscitation. Both documents serve to communicate a patient’s healthcare wishes, ensuring that their values guide medical decisions when they are unable to do so themselves.
Other Common State-specific Do Not Resuscitate Order Templates
What Is a Dnr Form - Education on DNRs can save families heartache by clarifying expectations during critical health crises.
For effective protection of confidential information, parties may consider utilizing resources like the smarttemplates.net to obtain a comprehensive New York Non-disclosure Agreement form, ensuring that their proprietary data remains secure and undisclosed in various business interactions.
Do Not Resuscitate Form Georgia - An individual’s personal beliefs and values can significantly influence their choice regarding a DNR.
Texas Ooh Dnr - Sometimes, a DNR order is included as part of a broader advance directive or living will.
More About Arizona Do Not Resuscitate Order
What is a Do Not Resuscitate (DNR) Order in Arizona?
A Do Not Resuscitate Order is a legal document that allows a person to refuse cardiopulmonary resuscitation (CPR) and other life-saving measures in the event of a medical emergency. In Arizona, this order must be signed by a physician and is intended to respect the wishes of individuals who do not wish to receive resuscitation efforts in specific situations.
Who can request a DNR Order?
Any adult who is capable of making their own medical decisions can request a DNR Order. This includes individuals with terminal illnesses, serious health conditions, or those who simply wish to avoid aggressive medical interventions at the end of life.
How is a DNR Order created in Arizona?
To create a DNR Order, a patient must discuss their wishes with their physician. The physician will then complete the Arizona DNR form, which must be signed by both the patient (or their legal representative) and the physician. It's important to keep copies of the signed form in accessible locations, such as with the patient’s medical records and with family members.
Where should I keep the DNR Order?
It is essential to keep the DNR Order in a place where it can be easily found in an emergency. Many people choose to keep it in their medical records or with their primary care physician. Others may carry a wallet card or wear a medical alert bracelet indicating their DNR status.
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time. The individual can verbally communicate their wish to revoke the order, or they can destroy the document. It’s advisable to inform healthcare providers and family members when the order is revoked to avoid any confusion during a medical emergency.
Does a DNR Order apply outside of a hospital setting?
Yes, a DNR Order is valid in both hospital and out-of-hospital settings in Arizona. However, it’s important to ensure that emergency medical personnel are aware of the DNR Order. This can often be done by displaying the DNR form prominently or having a designated person communicate the order in an emergency.
What happens if a DNR Order is not available during an emergency?
If a DNR Order is not available when emergency medical services arrive, the default action is to provide resuscitation. This is why having the DNR form readily accessible is crucial. It’s also beneficial to discuss your wishes with family members to ensure they understand and can communicate your preferences in an emergency.
Dos and Don'ts
When filling out the Arizona Do Not Resuscitate Order form, it’s important to follow certain guidelines to ensure your wishes are clearly expressed. Here are seven things to do and not to do:
- Do ensure that the form is completed in full. Every section must be filled out to avoid confusion.
- Do sign and date the form. Your signature confirms that the information is accurate and reflects your wishes.
- Do discuss your decision with your healthcare provider. They can provide guidance and help clarify any questions you may have.
- Do keep copies of the completed form. Distributing copies to your family and healthcare team ensures everyone is informed.
- Don't use outdated forms. Always use the most current version to ensure compliance with state regulations.
- Don't fill out the form under pressure. Take your time to think through your choices and discuss them with loved ones.
- Don't forget to review the form periodically. Your wishes may change, and it’s important to keep the document updated.
Arizona Do Not Resuscitate Order - Usage Steps
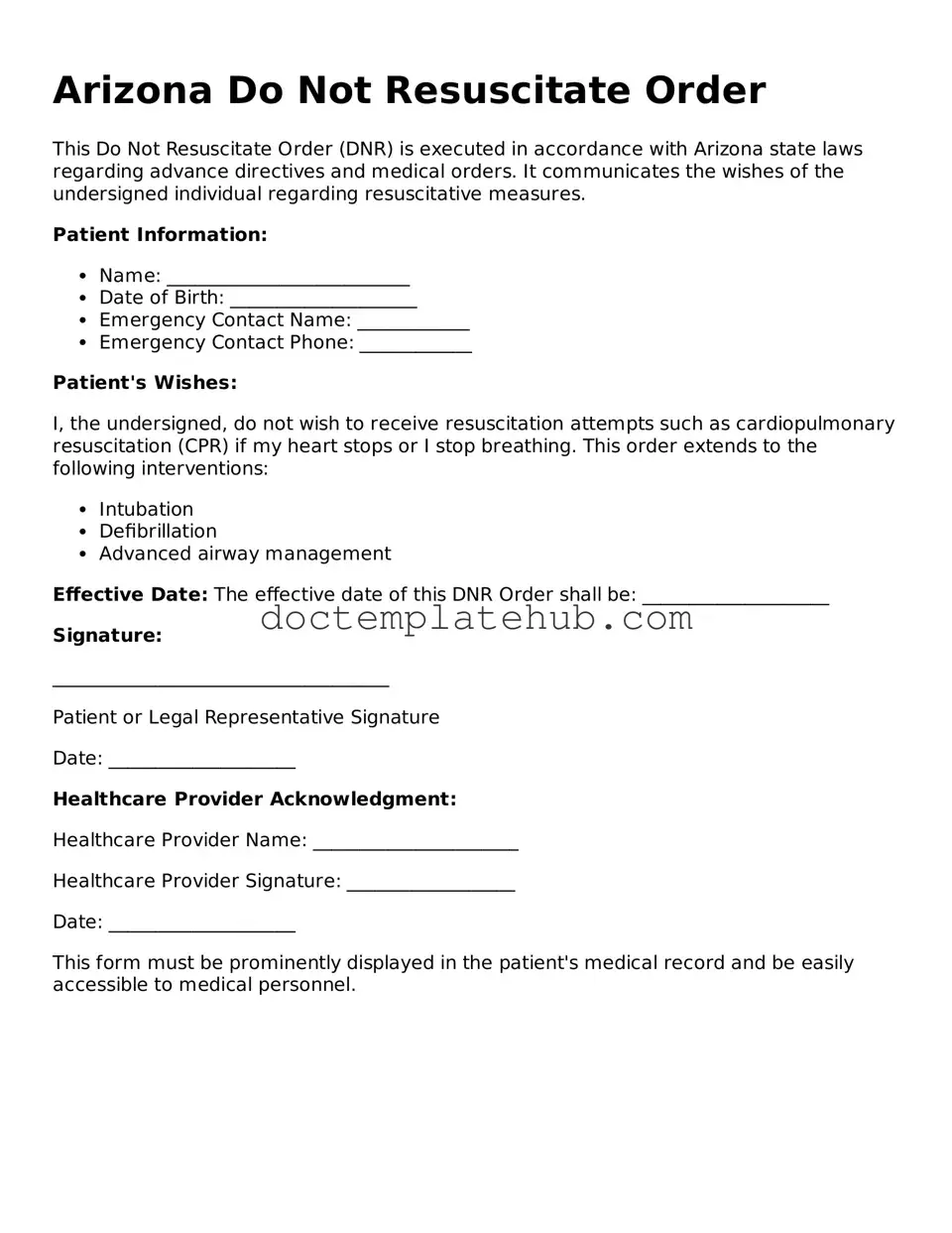
Filling out the Arizona Do Not Resuscitate Order form is an important step in expressing your healthcare wishes. This document ensures that your preferences regarding resuscitation are clearly communicated to medical professionals. Follow these steps to complete the form accurately.
- Obtain the Arizona Do Not Resuscitate Order form. You can find it online or request a copy from your healthcare provider.
- Begin by filling in your full name, date of birth, and address at the top of the form.
- Next, indicate whether you are the patient or the legal representative by checking the appropriate box.
- Provide the name of your physician and their contact information. This is important for verification purposes.
- Clearly state your wishes regarding resuscitation by checking the relevant boxes. Make sure you understand each option before making your selection.
- Sign and date the form at the designated area. If you are a legal representative, include your relationship to the patient.
- Have the form witnessed by two individuals who are not related to you and who will not benefit from your estate. They should sign and date the form as well.
- Make copies of the completed form for your records and share them with your healthcare provider and family members.
Once you have completed the form, keep it in a safe but accessible place. Make sure your loved ones know where it is located. It’s essential to communicate your wishes clearly, so everyone involved in your care understands your preferences.