Fillable Do Not Resuscitate Order Template for California State
The California Do Not Resuscitate (DNR) Order form serves as a crucial document for individuals who wish to express their preferences regarding medical interventions in the event of a life-threatening situation. This form is particularly significant for patients with terminal illnesses or those who are nearing the end of life, as it provides a clear directive to healthcare providers about the patient's wishes concerning resuscitation efforts. It outlines the specific circumstances under which resuscitation should not be performed, ensuring that the individual's desires are respected during critical moments. The DNR Order must be signed by both the patient and their physician, establishing a mutual understanding of the patient's medical condition and preferences. Additionally, the form is designed to be easily accessible and recognizable to medical personnel, which is vital in emergency situations. By completing this form, individuals can gain peace of mind, knowing that their healthcare choices will be honored, even when they may not be able to communicate them directly. Understanding the implications and processes involved in the DNR Order is essential for anyone considering this important aspect of end-of-life care.
Similar forms
The Advance Healthcare Directive is a legal document that allows individuals to outline their preferences for medical treatment in the event they become unable to communicate their wishes. Similar to the California Do Not Resuscitate Order (DNR), this directive can specify whether an individual wishes to receive resuscitation efforts or other life-sustaining treatments. It empowers individuals to make decisions about their healthcare in advance, ensuring that their wishes are honored even when they cannot speak for themselves.
The Physician Orders for Life-Sustaining Treatment (POLST) form serves a similar purpose by translating patient preferences into actionable medical orders. Like the DNR, the POLST form is intended for individuals with serious health conditions. It allows patients to specify their preferences regarding resuscitation and other life-sustaining measures, ensuring that healthcare providers follow these wishes in emergency situations.
The Living Will is another document that shares similarities with the DNR. This legal document allows individuals to express their wishes regarding end-of-life care. While the DNR specifically addresses resuscitation efforts, the Living Will encompasses a broader range of medical treatments, including artificial nutrition and hydration. Both documents aim to communicate patient preferences to healthcare providers and family members.
The Medical Power of Attorney (MPOA) enables an individual to designate someone to make healthcare decisions on their behalf if they become incapacitated. Similar to the DNR, this document ensures that a person’s healthcare preferences are respected. While the DNR focuses on resuscitation, the MPOA can cover a wide range of medical decisions, allowing the appointed individual to act in accordance with the patient’s wishes.
The Do Not Intubate (DNI) order is closely related to the DNR. It specifically instructs healthcare providers not to insert a breathing tube in the event of respiratory failure. While the DNR addresses cardiac arrest and resuscitation, the DNI focuses on situations where breathing assistance is required. Both documents are essential for guiding medical interventions in critical situations.
Understanding the significance of legal documents such as the Durable Power of Attorney is essential, as it grants a trusted individual the authority to make decisions on one's behalf, particularly concerning financial and legal matters. This arrangement is crucial for ensuring that the individual's wishes are respected, especially in situations where they may be incapacitated. Resources like smarttemplates.net can provide valuable information and templates to help individuals create these important documents effectively.
The Comfort Care Order emphasizes the provision of comfort and palliative care rather than curative treatment. This document aligns with the principles of the DNR by prioritizing quality of life over aggressive medical interventions. Patients who choose this option may wish to avoid resuscitation and instead receive supportive care to manage pain and discomfort.
The Do Not Hospitalize (DNH) order is designed for individuals who prefer to remain at home or in a non-hospital setting during a medical crisis. Like the DNR, the DNH reflects patient preferences regarding the level of care they wish to receive. This order can be particularly relevant for patients with terminal illnesses who seek to avoid hospitalization and its associated interventions.
The Out-of-Hospital Do Not Resuscitate (OOH DNR) order is similar to the California DNR but specifically applies to situations outside of a hospital setting. This document allows individuals to refuse resuscitation efforts in emergency situations, such as at home or in a nursing facility. It serves to communicate the patient’s wishes to emergency responders and healthcare providers in non-hospital environments.
The End-of-Life Care Plan is a comprehensive document that outlines an individual's wishes for care during their final days. It can include preferences regarding resuscitation, pain management, and other medical interventions. Similar to the DNR, this plan aims to ensure that healthcare providers respect the individual’s choices at the end of life, promoting a dignified and peaceful experience.
Other Common State-specific Do Not Resuscitate Order Templates
What Is a Dnr Form - The presence of a DNR can help reduce guilt or uncertainty for family members when medical decisions must be made.
What Are the 2 Types of Dnr? - All healthcare providers involved in a patient’s care should be aware of the existence of a DNR order.
Do Not Resuscitate Form Georgia - The DNR document addresses specific resuscitative measures, such as CPR and defibrillation.
A Doctors Excuse Note form serves as official documentation from a healthcare provider, confirming a patient's medical condition and the necessity for absence from work or school. This note can be essential for ensuring that employees and students receive the appropriate accommodations during their recovery. For more information on obtaining a template for this form, you can visit https://documentonline.org/blank-doctors-excuse-note/. Understanding its importance can help individuals navigate their healthcare and employer policies effectively.
Dnr Directive - Understanding a DNR is critical for effective patient-provider communication.
More About California Do Not Resuscitate Order
What is a Do Not Resuscitate (DNR) Order in California?
A Do Not Resuscitate Order is a legal document that allows individuals to refuse cardiopulmonary resuscitation (CPR) and other life-saving measures in the event of cardiac arrest or respiratory failure. In California, this order is intended for patients who wish to avoid aggressive medical interventions at the end of life.
Who can request a DNR Order?
In California, a DNR Order can be requested by adults who are capable of making their own medical decisions. This includes individuals who are diagnosed with a terminal illness or have a medical condition that significantly limits their life expectancy. Additionally, a legally authorized representative, such as a healthcare proxy, may also request a DNR on behalf of an incapacitated person.
How do I obtain a DNR Order in California?
To obtain a DNR Order, you must fill out the California Do Not Resuscitate form. This form can typically be acquired through healthcare providers, hospitals, or online resources. After completing the form, it must be signed by both the patient and their physician to be valid. It is crucial to keep the signed form in a location that is easily accessible to emergency medical personnel.
What should I do with the DNR Order once it is completed?
Once the DNR Order is completed and signed, it is important to keep it in a visible place, such as on the refrigerator or in a medical file. Inform family members, friends, and healthcare providers about the existence of the DNR Order. This ensures that everyone involved in your care understands your wishes regarding resuscitation.
Can a DNR Order be revoked?
Yes, a DNR Order can be revoked at any time by the individual who created it. This can be done verbally or by destroying the original document. It is advisable to inform healthcare providers and family members of the revocation to prevent any confusion during medical emergencies.
Will a DNR Order affect other medical treatments?
A DNR Order specifically addresses resuscitation efforts and does not affect other medical treatments. Patients can still receive necessary medical care, including pain management and other supportive treatments, even if they have a DNR Order in place. It is essential to discuss your overall treatment preferences with your healthcare team.
What happens if I do not have a DNR Order?
If you do not have a DNR Order and experience a medical emergency, healthcare providers are required to perform resuscitation efforts unless there is a clear indication of a patient's wishes otherwise. This may result in unwanted aggressive interventions, which may not align with your preferences regarding end-of-life care.
Can I change my mind about a DNR Order?
Absolutely. Individuals have the right to change their mind about a DNR Order at any time. If you decide to modify your preferences, it is essential to create a new DNR Order and communicate this change to your healthcare providers and loved ones to ensure your current wishes are respected.
Dos and Don'ts
When filling out the California Do Not Resuscitate Order form, it is important to follow certain guidelines to ensure the document is completed correctly. Here are five things to do and five things to avoid.
Things You Should Do:
- Read the instructions carefully before starting.
- Provide clear and accurate information about the patient.
- Sign and date the form where required.
- Discuss the decision with family members and healthcare providers.
- Keep a copy of the completed form for personal records.
Things You Shouldn't Do:
- Do not leave any required fields blank.
- Do not use unclear or ambiguous language.
- Do not sign the form without understanding its implications.
- Do not forget to inform emergency medical personnel about the order.
- Do not assume that verbal instructions are sufficient; always use the form.
California Do Not Resuscitate Order - Usage Steps
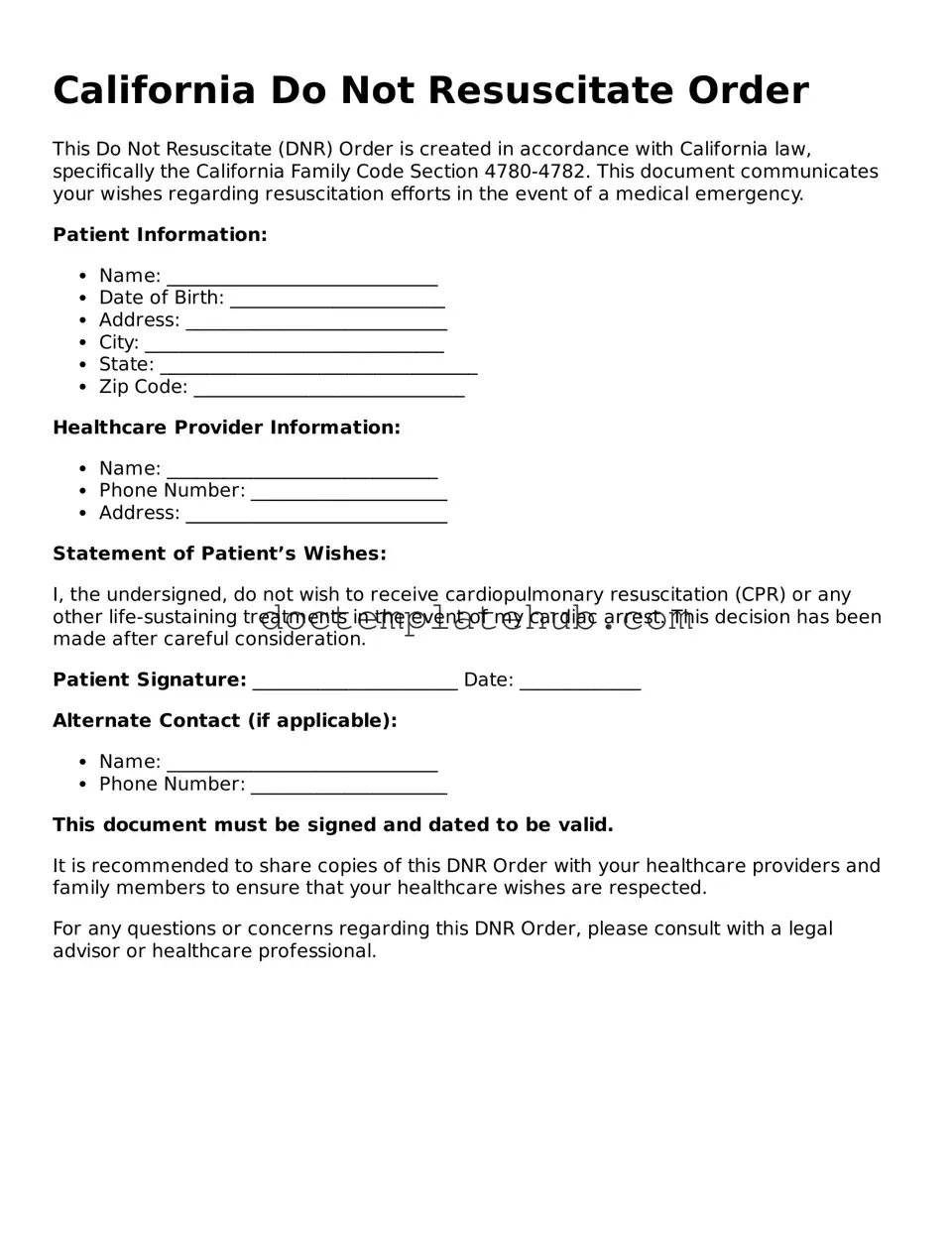
Filling out the California Do Not Resuscitate Order form is an important step in expressing your healthcare preferences. This document allows you to communicate your wishes regarding resuscitation efforts in the event of a medical emergency. Follow these steps to complete the form accurately.
- Obtain the California Do Not Resuscitate Order form. You can find it online or request a copy from your healthcare provider.
- Carefully read the instructions included with the form to ensure you understand the requirements.
- Fill in your full name, date of birth, and address at the top of the form.
- Indicate the date you are completing the form.
- Sign the form in the designated area. This signature confirms your wishes.
- Have your signature witnessed by two individuals. They should not be related to you or your healthcare provider.
- Make a copy of the completed form for your records.
- Provide copies of the signed form to your healthcare provider and any family members involved in your care.