Fill Your Cna Shower Sheets Form
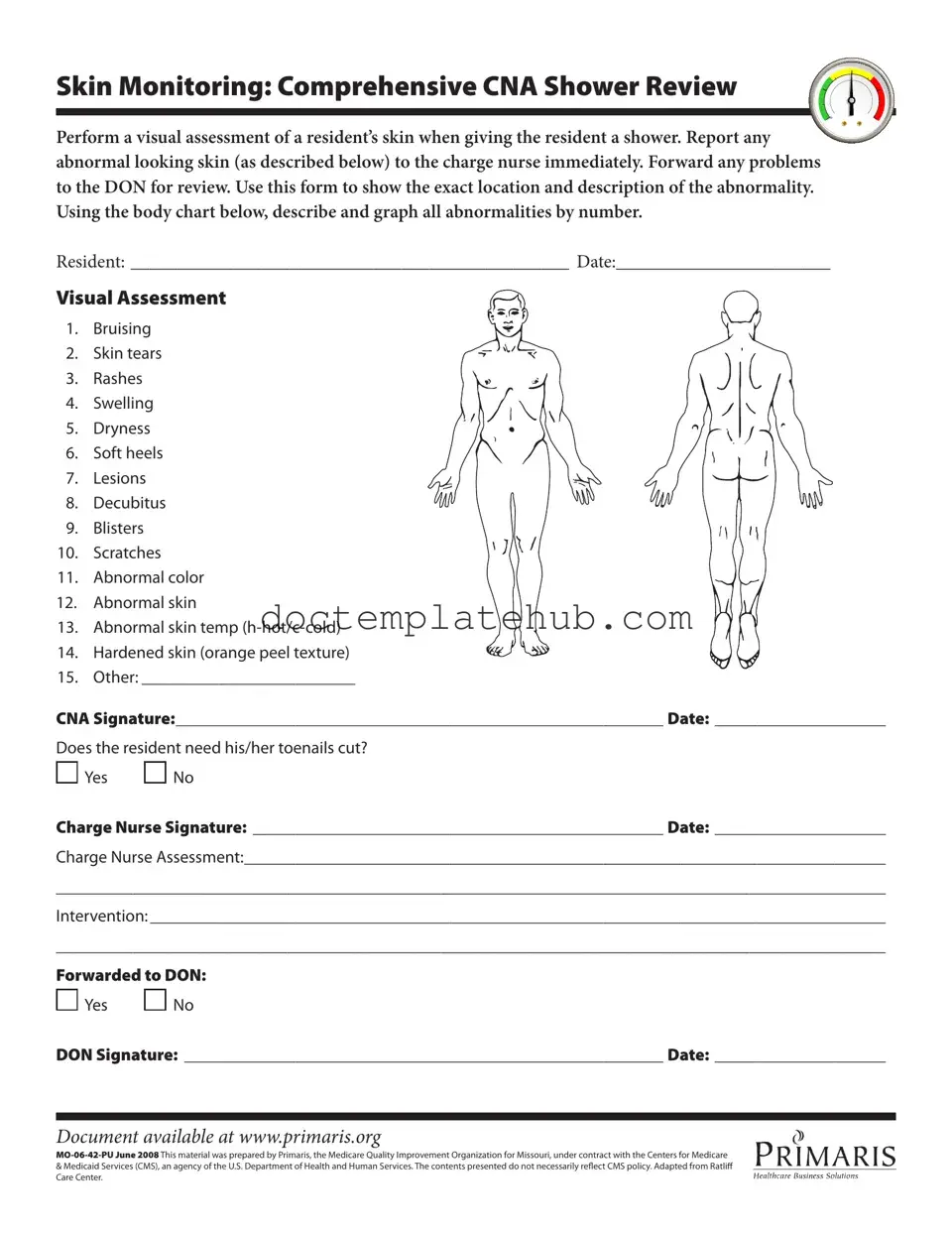
The CNA Shower Sheets form plays a crucial role in ensuring the health and safety of residents during bathing. This form is designed for Certified Nursing Assistants (CNAs) to conduct a thorough visual assessment of a resident's skin while providing a shower. It emphasizes the importance of identifying any abnormalities, such as bruising, skin tears, rashes, or lesions, and mandates that these findings be reported immediately to the charge nurse. The form includes a body chart for CNAs to accurately document the location and description of any skin issues. This systematic approach not only aids in monitoring skin health but also facilitates communication among healthcare staff. The process requires the CNA to sign the form, indicating their observations, and includes a section for the charge nurse to assess the situation further. Additionally, it addresses the need for toenail care, ensuring that all aspects of the resident's personal hygiene are considered. This comprehensive documentation is vital for ongoing care and is forwarded to the Director of Nursing (DON) for review when necessary, reinforcing a commitment to high standards of resident care.
Similar forms
The CNA Shower Sheets form is similar to the Resident Assessment Protocol (RAP) form, which is used to evaluate various aspects of a resident's health and well-being. Both documents require a detailed observation of the resident's condition. While the CNA Shower Sheets focus specifically on skin assessments during bathing, the RAP form covers a broader range of health indicators. Both forms emphasize the importance of reporting any abnormalities to the appropriate nursing staff for further evaluation and care.
Another document that shares similarities is the Daily Care Log. This log is used by nursing staff to document the daily care provided to each resident. Like the CNA Shower Sheets, it includes sections for noting any changes in the resident’s condition. Both documents serve as important communication tools among staff, ensuring that any issues are promptly addressed and that care is consistent and thorough.
The Skin Integrity Assessment form is also comparable to the CNA Shower Sheets. This form is specifically designed to monitor and document the condition of a resident’s skin over time. It includes similar categories for assessing skin issues such as rashes, bruises, and lesions. Both documents aim to ensure that any skin problems are identified early and that appropriate interventions are implemented to maintain skin health.
The Incident Report form bears resemblance to the CNA Shower Sheets in that it is used to document any unusual occurrences or changes in a resident's health status. While the CNA Shower Sheets focus on skin assessments during showers, the Incident Report provides a broader context for any incidents that may affect a resident's well-being. Both forms require timely reporting and follow-up to ensure that proper care is provided.
The Care Plan form is another document that aligns with the CNA Shower Sheets. Care Plans are developed based on assessments of a resident’s needs, including skin care. Both documents require input from nursing staff and emphasize the importance of personalized care. The CNA Shower Sheets provide specific observations that can inform updates to the Care Plan, ensuring that skin issues are adequately addressed.
Understanding the significance of thorough documentation in patient care is essential, particularly when considering the importance of legal documents like the Texas Last Will and Testament. Just as the Patient Assessment Tool and other forms ensure a comprehensive overview of a patient's health and treatment needs, having a well-drafted will ensures that an individual's final wishes regarding their assets are followed. For those looking to create a Last Will and Testament, resources available at smarttemplates.net can provide valuable guidance in navigating this important legal process.
The Nursing Progress Notes are similar in purpose to the CNA Shower Sheets. These notes document ongoing observations and assessments of a resident's condition. While the CNA Shower Sheets focus specifically on skin assessments during showering, Nursing Progress Notes capture a broader range of observations. Both documents are essential for maintaining a comprehensive view of a resident’s health and for facilitating effective communication among care team members.
The Admission Assessment form also shares similarities with the CNA Shower Sheets. This form is completed when a resident first enters a facility and includes a thorough evaluation of their health status. Like the CNA Shower Sheets, it includes sections for documenting skin conditions and other health concerns. Both forms are crucial for establishing a baseline for care and ensuring that any issues are promptly addressed.
The Medication Administration Record (MAR) is another document that has some parallels with the CNA Shower Sheets. While the MAR focuses on the administration of medications, it also requires documentation of any side effects or reactions that may affect a resident's skin or overall health. Both documents emphasize the importance of careful monitoring and reporting to ensure the safety and well-being of residents.
Lastly, the Fall Risk Assessment form is similar to the CNA Shower Sheets in that both documents evaluate aspects of a resident's physical condition that could impact their safety. While the Fall Risk Assessment focuses on mobility and balance, the CNA Shower Sheets assess skin integrity during bathing. Both forms contribute to a comprehensive understanding of a resident’s needs and help inform care strategies to prevent injuries.
Other PDF Templates
Set Up March Madness Bracket - Be mindful of matchups as they can impact game outcomes.
In order to take the necessary steps when addressing lease violations, landlords may find it helpful to download the document in pdf, which outlines the process and requirements involved in issuing a Florida Notice to Quit. This ensures that all procedures are followed correctly and that both the landlord and tenant are aware of their rights and responsibilities throughout the eviction process.
Free Printable Puppy Shot Record - Streamline process and paperwork by using this comprehensive vaccination form.
Health Insurance Marketplace Statement - The form includes a specific section where taxpayers can report how many months they were enrolled in coverage.
More About Cna Shower Sheets
What is the purpose of the CNA Shower Sheets form?
The CNA Shower Sheets form is designed to help Certified Nursing Assistants (CNAs) perform a thorough visual assessment of a resident’s skin during shower time. By documenting any abnormalities, such as bruises, rashes, or lesions, the form ensures that these issues are reported to the charge nurse promptly. This process not only enhances the resident's care but also helps maintain a high standard of health monitoring within the facility.
How should I document skin abnormalities on the form?
When documenting skin abnormalities, you should first conduct a careful visual assessment of the resident's skin. Use the body chart provided on the form to mark the exact location of any issues. For each abnormality, describe it in detail, referring to the list of conditions such as swelling, dryness, or abnormal color. Be as specific as possible to ensure that the charge nurse and Director of Nursing (DON) can understand the situation clearly.
What should I do if I notice an abnormality during the assessment?
If you notice any abnormalities while assessing the resident's skin, it is crucial to report them to the charge nurse immediately. This step is vital for ensuring that the resident receives the appropriate care. After reporting, you should also forward any concerns to the DON for further review. Documenting your observations accurately on the form will facilitate effective communication among the healthcare team.
Is there a section for additional comments or interventions on the form?
Yes, the CNA Shower Sheets form includes sections for the charge nurse's assessment and any recommended interventions. After you complete your initial assessment, the charge nurse will review your findings and may add their observations. This collaborative approach helps ensure that all aspects of the resident’s care are addressed. If necessary, the form also allows for documentation of whether the issue has been forwarded to the DON for further action.
Dos and Don'ts
When filling out the CNA Shower Sheets form, it's essential to follow specific guidelines to ensure accuracy and clarity. Here’s a helpful list of things to do and avoid:
- Do perform a thorough visual assessment of the resident's skin during the shower.
- Do report any abnormalities immediately to the charge nurse.
- Do use the body chart to accurately describe and graph any skin issues.
- Do ensure the resident's name and date are clearly written on the form.
- Do sign and date the form to confirm your observations and actions.
- Do forward any concerns to the Director of Nursing (DON) for further review.
- Don't skip any areas during the skin assessment; every part of the body matters.
- Don't use vague language when describing abnormalities; be as specific as possible.
- Don't forget to check if the resident needs toenail care; this is an important part of their hygiene.
- Don't leave any sections of the form blank; incomplete forms can lead to misunderstandings.
- Don't hesitate to ask for clarification if you are unsure about any part of the form.
- Don't overlook the need for the charge nurse's signature; it is a crucial step in the process.
Cna Shower Sheets - Usage Steps
After completing the CNA Shower Sheets form, it will be used to document skin assessments during resident showers. This process ensures any abnormalities are noted and communicated to the appropriate personnel for further action. Follow these steps to accurately fill out the form.
- Write the resident's name in the designated space labeled RESIDENT:.
- Enter the date of the assessment in the DATE: section.
- Perform a visual assessment of the resident's skin during the shower.
- Identify any abnormalities using the provided list and mark the corresponding numbers on the body chart.
- In the space for Other:, describe any additional abnormalities not listed.
- Sign the form in the CNA Signature: section and add the date.
- Indicate whether the resident needs toenails cut by marking Yes or No.
- Have the charge nurse sign in the Charge Nurse Signature: section and record the date.
- Provide a brief assessment in the Charge Nurse Assessment: area.
- Outline any interventions in the Intervention: section.
- Note if the form has been forwarded to the Director of Nursing (DON) by marking Yes or No.
- Have the DON sign in the DON Signature: section and include the date.