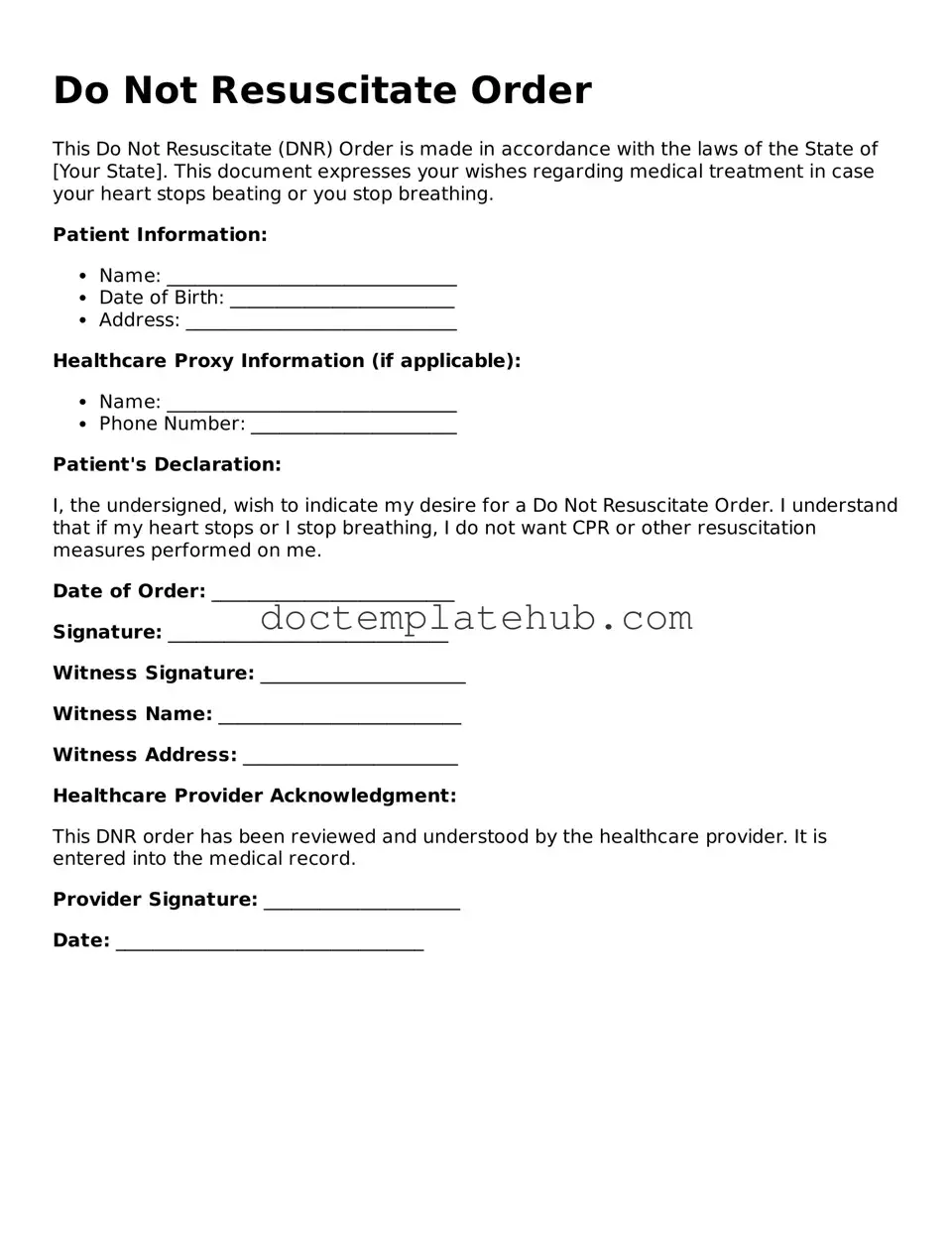
Official Do Not Resuscitate Order Form
When it comes to making crucial healthcare decisions, understanding the Do Not Resuscitate (DNR) Order form is essential for patients and their families. This legal document allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency where their heart or breathing stops. The DNR Order form typically includes vital information such as the patient's name, date of birth, and the signature of the patient or their authorized representative. It serves as a clear directive to healthcare providers, ensuring that the patient's preferences are respected during critical moments. Additionally, the form may require the involvement of a physician, who must confirm that the patient is fully informed about the implications of the order. By understanding the intricacies of the DNR Order form, individuals can make empowered choices that reflect their values and desires regarding end-of-life care, fostering open discussions with loved ones and medical professionals alike.
Similar forms
A Living Will is a document that outlines a person's wishes regarding medical treatment in situations where they can no longer communicate. Like a Do Not Resuscitate Order (DNR), a Living Will provides guidance to healthcare providers about the types of medical interventions a patient desires or wishes to avoid. This document typically addresses end-of-life care and can include decisions about life support, pain management, and other critical medical treatments. Both documents serve to ensure that a patient's preferences are respected, especially in emergencies.
A Healthcare Power of Attorney (POA) allows individuals to designate someone to make medical decisions on their behalf if they become incapacitated. Similar to a DNR, a Healthcare POA ensures that a person's healthcare preferences are honored. While a DNR specifically addresses resuscitation efforts, a Healthcare POA can cover a broader range of medical decisions. This document empowers a trusted individual to act in accordance with the patient’s wishes, providing peace of mind that their choices will be respected even when they cannot voice them.
In the context of protecting sensitive business information, it is crucial to understand the importance of a Utah Non-disclosure Agreement form. This legally binding document helps to prevent the unauthorized sharing of confidential details, particularly during significant business dealings. To find templates for drafting such agreements, you can visit smarttemplates.net, where resources are available tailored to your specific needs.
An Advance Directive combines elements of both a Living Will and a Healthcare Power of Attorney. It allows individuals to specify their medical treatment preferences and appoint someone to make decisions for them. Like a DNR, an Advance Directive is crucial for guiding healthcare providers in respecting a patient's wishes. This comprehensive document can address various scenarios, from end-of-life care to specific treatments, ensuring that a person's values and preferences are honored in any medical situation.
A Comfort Care Order focuses on ensuring that a patient receives comfort measures rather than aggressive treatments. Like a DNR, it emphasizes the importance of quality of life over invasive procedures. This document may include instructions for pain management, emotional support, and other palliative care options. While a DNR prevents resuscitation, a Comfort Care Order prioritizes the patient's comfort and dignity during the dying process, making it a vital component of end-of-life care planning.
Common Forms
Streamlined Foreign Offshore Procedures - Failure to respond to every section of Form 14653 may delay processing and compliance eligibility.
The Employee Handbook form serves as an essential document that outlines a company's policies, procedures, and expectations for its employees. It provides guidance on various topics, including workplace behavior, benefits, and compliance with workplace laws. For a useful template, you can refer to https://documentonline.org/blank-employee-handbook. Having a comprehensive and clear handbook can help both employees and employers understand their rights and responsibilities within the organization.
Declaration of Residency - An Affidavit of Residency is a legal document that confirms an individual's address.
Asylum Uscis - Completing the I-589 is a critical step for those facing danger at home.
More About Do Not Resuscitate Order
What is a Do Not Resuscitate Order (DNR) form?
A Do Not Resuscitate Order (DNR) form is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. When a person has a DNR in place, medical personnel are instructed not to perform cardiopulmonary resuscitation (CPR) or other life-saving measures if the individual stops breathing or their heart stops beating. This order is typically used by individuals with terminal illnesses or severe health conditions who wish to avoid aggressive interventions that may not improve their quality of life.
Who can complete a DNR order?
A DNR order can be completed by a competent adult who understands the implications of the document. This may include patients themselves or, in some cases, legal representatives or healthcare proxies if the patient is unable to make decisions. It is essential for individuals to discuss their wishes with family members and healthcare providers to ensure that everyone understands the intent behind the DNR order. In some states, specific forms or procedures may be required to validate the DNR, so consulting with a healthcare professional is advisable.
How is a DNR order implemented in a healthcare setting?
Once a DNR order is completed and signed, it should be provided to all healthcare providers involved in the individual’s care. This includes hospitals, nursing homes, and emergency medical services. The order is typically placed in the patient's medical record and should be easily accessible to medical staff. In emergency situations, first responders will look for the DNR order to determine the appropriate course of action. It is crucial for individuals with a DNR order to carry a copy with them, especially if they are traveling or may be in situations where emergency care is needed.
Can a DNR order be revoked or changed?
Yes, a DNR order can be revoked or changed at any time by the individual who signed it. To do so, the individual should clearly communicate their wishes to their healthcare provider and ensure that any new directives are documented appropriately. It is also advisable to inform family members and caregivers about the changes to avoid confusion during a medical emergency. If a person decides to cancel their DNR, they should destroy any copies of the original document to prevent any miscommunication in the future.
Dos and Don'ts
When filling out a Do Not Resuscitate (DNR) Order form, it is important to follow certain guidelines to ensure clarity and compliance. Below is a list of actions to take and avoid.
- Do clearly state your wishes regarding resuscitation.
- Do discuss your decision with your healthcare provider.
- Do ensure that the form is signed and dated.
- Do keep copies of the completed form in accessible locations.
- Don't use vague language that could lead to confusion.
- Don't fill out the form without consulting with family or medical professionals.
- Don't forget to review and update the form as needed.
- Don't assume that verbal instructions are sufficient; written documentation is essential.
Do Not Resuscitate Order - Usage Steps
Completing a Do Not Resuscitate Order (DNR) form is an important step in expressing your healthcare preferences. After filling out the form, it should be signed and dated, then shared with your healthcare provider to ensure your wishes are known and respected.
- Obtain a blank DNR form from your healthcare provider or download it from a reputable source.
- Fill in your full name, date of birth, and any other identifying information required on the form.
- Clearly indicate your wishes regarding resuscitation by checking the appropriate box or writing your preference in the designated area.
- Include the date on which you are completing the form.
- Sign the form to validate your wishes. If you are unable to sign, a designated representative may sign on your behalf.
- Have a witness sign the form, if required by your state’s regulations.
- Make copies of the completed form for your healthcare provider, family members, and keep one for your records.
- Discuss your DNR order with your healthcare provider to ensure it is properly documented in your medical records.