Fill Your Medication Administration Record Sheet Form
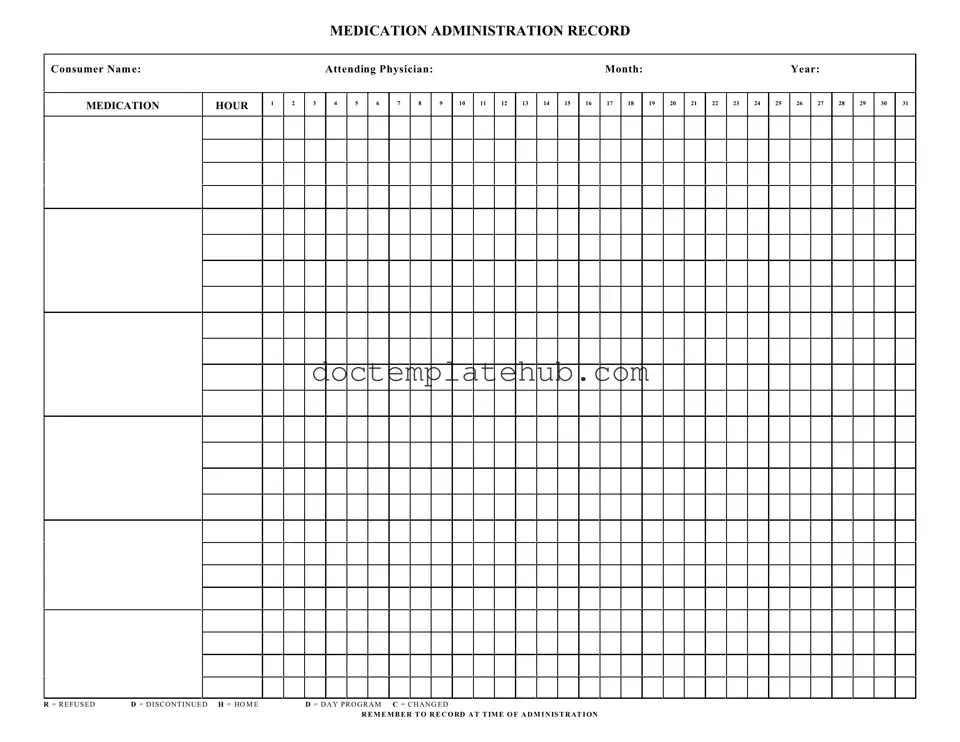
The Medication Administration Record Sheet (MARS) is an essential tool in healthcare settings, facilitating the accurate tracking of medication administration for patients. This form captures crucial details, including the consumer's name, the attending physician, and the specific month and year of medication administration. Each hour of the day is meticulously laid out, allowing healthcare providers to document medication given at various times. The form includes specific notations, such as "R" for refused, "D" for discontinued, "H" for home, "D" for day program, and "C" for changed, which help in maintaining clear communication about the patient's medication regimen. By ensuring that all entries are recorded at the time of administration, the MARS promotes accountability and helps prevent medication errors, ultimately enhancing patient safety and care quality. This structured approach to medication management is vital in both residential and outpatient settings, where adherence to prescribed therapies can significantly impact health outcomes.
Similar forms
The Medication Administration Record (MAR) is similar to the Patient Medication Profile. Both documents serve to track the medications prescribed to an individual. The Patient Medication Profile provides a comprehensive overview of a patient's medication history, including dosages and administration times. This profile is often utilized by healthcare providers to ensure that patients receive the correct medications at the appropriate times, similar to how the MAR records actual administration events and any refusals or changes in medication. By maintaining an accurate record, both documents contribute to patient safety and effective medication management.
Another document that shares similarities with the MAR is the Medication Reconciliation Form. This form is used to compare a patient's current medications with those that were previously prescribed. The goal is to identify any discrepancies and ensure that the patient’s medication list is accurate. Like the MAR, the Medication Reconciliation Form emphasizes the importance of accuracy in medication administration. Both documents require careful attention to detail and serve as vital tools in preventing medication errors during transitions of care, such as hospital admissions or discharges.
The importance of maintaining accurate documentation in healthcare cannot be overstated, as it relates directly to patient safety and quality of care. Whether utilizing forms like the Medication Administration Record Sheet or the Nursing Medication Flow Sheet, healthcare professionals must rely on comprehensive tools to ensure precision in medication administration. For additional resources regarding essential documentation like the Straight Bill Of Lading form, you can visit smarttemplates.net.
Lastly, the Nursing Care Plan bears similarities to the MAR in that both documents are integral to patient care. The Nursing Care Plan outlines the specific nursing interventions and goals for a patient, including medication administration as a key component. While the MAR records the actual administration of medications, the Nursing Care Plan provides the context for why those medications are being given. Both documents work in tandem to ensure that nursing staff are aware of the patient’s needs and the prescribed treatment regimen, thereby promoting a coordinated approach to patient care.
Other PDF Templates
Better Business Bureau Complaint - Share your thoughts on how a company handled an emergency smoothly.
A Doctors Excuse Note form serves as official documentation from a healthcare provider, confirming a patient's medical condition and the necessity for absence from work or school. This note can be essential for ensuring that employees and students receive the appropriate accommodations during their recovery. Understanding its importance can help individuals navigate their healthcare and employer policies effectively. For more information, you can refer to the following resource: https://documentonline.org/blank-doctors-excuse-note.
Aia Statement of Qualifications - It is a key part of many contractors’ marketing toolkit.
Constellation Bracket - Success in the consolation bracket can serve as a springboard for future competitions.
More About Medication Administration Record Sheet
What is the purpose of the Medication Administration Record Sheet?
The Medication Administration Record Sheet (MARS) is designed to track the administration of medications to consumers. It ensures that medications are given at the correct times and helps monitor any changes in the medication regimen.
How should I fill out the consumer's name on the form?
Clearly write the consumer's full name at the top of the form. This helps ensure that the medication records are accurate and linked to the correct individual.
What information is required in the 'Attending Physician' section?
In the 'Attending Physician' section, include the name of the physician responsible for the consumer's care. This allows for quick reference in case of any questions or concerns regarding the medication prescribed.
How do I indicate that a medication was refused?
If a consumer refuses medication, mark the appropriate time slot with an "R" to indicate refusal. This notation is crucial for tracking compliance and understanding the consumer's medication history.
What does it mean if a medication is marked as discontinued?
Marking a medication with a "D" signifies that it has been discontinued. This helps keep the record up to date and prevents confusion about medications that are no longer being administered.
How can I indicate a change in medication on the form?
Use the letter "C" to denote a change in medication. Ensure that the new medication details are recorded accurately in the appropriate section of the form to maintain clarity.
What should I do if I administer a medication outside the scheduled hour?
In cases where a medication is administered outside the scheduled hour, document the time of administration clearly. This is important for maintaining accurate records and ensuring the consumer's safety.
How do I record medications administered during a day program?
If medications are administered during a day program, use the letter "D" to indicate this on the form. This helps differentiate between medications given at home and those given in a program setting.
What happens if I forget to record a medication administration?
It's essential to record each administration at the time it occurs. If you forget, make a note as soon as you remember. Consistent record-keeping is vital for the consumer's health and safety.
Why is it important to record the time of administration?
Recording the time of administration is crucial for tracking medication effectiveness and ensuring that doses are spaced appropriately. This information helps healthcare providers make informed decisions about the consumer's care.
Dos and Don'ts
When filling out the Medication Administration Record Sheet form, it’s important to follow best practices to ensure accuracy and compliance. Here are ten things to keep in mind:
- Do write clearly and legibly to avoid any misunderstandings.
- Do use the correct consumer name and ensure it matches their medical records.
- Do record the medication administration time accurately.
- Do mark any refusals or changes clearly using the designated codes.
- Do double-check the medication dosage before administration.
- Don't leave any blank spaces on the form; fill in all required fields.
- Don't use abbreviations that could lead to confusion.
- Don't forget to date and sign the record after completing the medication administration.
- Don't alter or erase any information once it has been written.
- Don't share the form with unauthorized personnel; maintain confidentiality.
Following these guidelines will help ensure that the Medication Administration Record Sheet is filled out correctly and efficiently.
Medication Administration Record Sheet - Usage Steps
Completing the Medication Administration Record Sheet is an important task that ensures accurate tracking of medication given to individuals. This form helps maintain a clear record of when and how medications are administered, as well as any changes or refusals. Follow these steps to fill out the form correctly.
- Start by entering the Consumer Name at the top of the form.
- Next, fill in the Attending Physician's name.
- Indicate the Month and Year for the record you are completing.
- For each day of the month, locate the corresponding box under the appropriate hour.
- Record the medication administration by entering the dose given in the box for that specific hour and day.
- If the medication was refused, write an R in the box.
- If the medication was discontinued, use a D.
- For medications that were given at home, mark an H.
- Use D for medications administered during a day program.
- If there was a change in the medication, indicate this with a C.
- Make sure to record the time of administration accurately in the designated area.