Fill Your Progress Notes Form
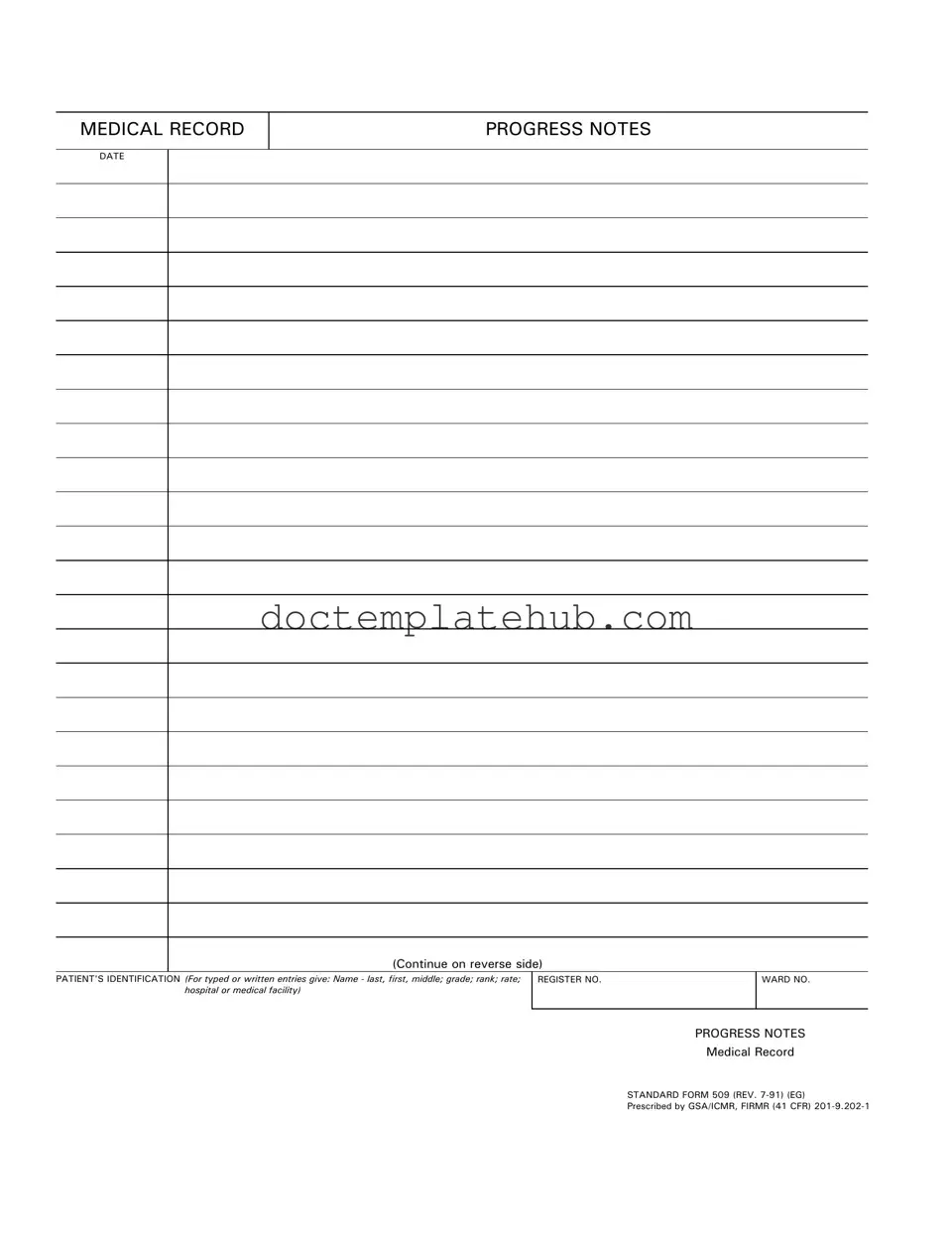
The Progress Notes form serves as a vital component in the documentation of patient care within medical records. This form captures essential information about a patient's treatment, ensuring that healthcare providers maintain a comprehensive record of the patient's progress over time. It includes fields for the patient's identification, which requires details such as the name—last, first, and middle—along with their grade, rank, rate, and the specific hospital or medical facility where they are receiving care. The date of each entry is crucial, as it provides a timeline of the patient's medical history and ongoing treatment. Standard Form 509, revised in July 1991, is the designated format for these notes, prescribed by the General Services Administration and the Information Collection Management Regulations. By adhering to this standardized form, healthcare professionals can ensure consistency and clarity in the documentation process, facilitating better communication among medical staff and improving the overall quality of patient care.
Similar forms
The first document similar to the Progress Notes form is the Patient Encounter Form. This form captures the details of a patient's visit, including the reason for the visit, the services provided, and any follow-up instructions. Like Progress Notes, it serves as a record of the patient's medical history and treatment plan, ensuring continuity of care. Both documents are essential for healthcare providers to track patient progress and make informed decisions regarding future treatments.
The second document is the Treatment Plan. This document outlines the specific goals and interventions for a patient's care. It is similar to Progress Notes in that it provides a structured approach to managing a patient's condition. Both documents require updates as the patient's situation changes, allowing healthcare providers to adjust their strategies accordingly. This ensures that care remains aligned with the patient's needs and progress.
The New York Promissory Note document is designed to formally represent the obligation of a borrower to repay a designated amount of money to a lender. Such a form is vital in defining the terms of the loan agreement, helping both parties understand their rights and responsibilities. For more information, you can refer to the detailed Promissory Note guidelines.
The third document is the Discharge Summary. This summary is created when a patient is discharged from a healthcare facility. It includes information about the patient's condition at discharge, treatments received, and follow-up care instructions. Like Progress Notes, it serves to communicate vital information among healthcare providers and ensures that the patient continues to receive appropriate care after leaving the facility.
The fourth document is the Clinical Assessment. This assessment evaluates a patient's health status and includes findings from physical exams, lab tests, and imaging studies. Similar to Progress Notes, it documents clinical observations and informs treatment decisions. Both documents are crucial for maintaining accurate and comprehensive medical records that reflect the patient's health over time.
The fifth document is the Medication Administration Record (MAR). The MAR tracks all medications administered to a patient during their stay. It shares similarities with Progress Notes in that it provides a chronological account of care and is used to monitor patient responses to medications. Both documents are vital for ensuring patient safety and adherence to prescribed treatments.
The sixth document is the Referral Form. This form is used when a healthcare provider refers a patient to a specialist. It includes pertinent patient information and the reason for the referral. Like Progress Notes, it ensures that all relevant information is communicated effectively, facilitating coordinated care among different providers and specialists.
The seventh document is the Consent Form. This form records a patient's agreement to undergo specific treatments or procedures. It is similar to Progress Notes in that it captures essential information about the patient's treatment journey. Both documents help protect patient rights and ensure that they are informed about their care options.
The eighth document is the Follow-Up Note. This note is used to document a patient's progress after a previous visit or treatment. It shares similarities with Progress Notes by providing updates on the patient's condition and any new developments. Both documents are essential for evaluating treatment effectiveness and making necessary adjustments to the care plan.
Other PDF Templates
Financial Affidavit Short Form Florida - Use the form as a tool to represent your financial needs clearly.
When considering the creation of a Power of Attorney in Texas, it's important to consult reliable resources to better understand the process and necessary documentation. For comprehensive guidance, you might want to visit smarttemplates.net, which provides valuable templates and information to assist you in drafting an effective Power of Attorney form tailored to your needs.
How to Add Money to Netspend Card - Contacting the merchant may help resolve disputes more efficiently.
More About Progress Notes
What is the purpose of the Progress Notes form?
The Progress Notes form is used to document patient care and treatment within medical facilities. It serves as a record of the patient's medical history, ongoing treatment, and any changes in their condition. This documentation is crucial for ensuring continuity of care and effective communication among healthcare providers.
What information is required on the Progress Notes form?
Essential information includes the patient's identification, such as their name (last, first, middle), grade, rank, rate, and the medical facility or hospital name. Additionally, the date of the notes must be recorded. This information helps to accurately track the patient's medical history and treatment progress.
How should I fill out the Progress Notes form?
When completing the form, ensure that all required fields are filled out clearly. Use either typed or handwritten entries, making sure that the handwriting is legible. Document the date at the top and provide detailed notes regarding the patient's condition, treatments administered, and any observations made during the visit.
Can I continue my notes on the back of the form?
Yes, you can continue your notes on the back of the Progress Notes form. If more space is needed to document the patient's progress, use the reverse side to ensure that all relevant information is captured. This helps maintain a comprehensive record of the patient's care.
What should I do if I make a mistake on the Progress Notes form?
If you make a mistake, do not attempt to erase or cover it up. Instead, cross out the error neatly and write the correct information next to it. Initial the correction to indicate that it was made by you. This practice maintains the integrity of the medical record while ensuring accuracy.
Is the Progress Notes form standardized?
Yes, the Progress Notes form is a standardized document, specifically the Standard Form 509 (REV. 7-91). It is prescribed by the General Services Administration (GSA) and follows specific guidelines to ensure consistency across medical records. Using a standardized form helps facilitate better communication and record-keeping in healthcare settings.
Dos and Don'ts
When filling out the Progress Notes form, it's important to adhere to certain guidelines to ensure accuracy and clarity. Here are seven things you should and shouldn't do:
- Do provide the patient's full name, including last, first, and middle names.
- Do include the patient's grade, rank, and rate as applicable.
- Do accurately fill in the date of the progress notes.
- Do ensure that the identification information is clearly legible, whether typed or handwritten.
- Don't omit the register number and ward number; these are critical for record keeping.
- Don't use abbreviations or shorthand that may confuse the reader.
- Don't forget to check for any errors before submitting the form.
By following these guidelines, you can help maintain the integrity of the medical record and ensure that all necessary information is properly documented.
Progress Notes - Usage Steps
Completing the Progress Notes form is an essential step in documenting patient care. This form captures important information about the patient's condition and treatment. Follow these steps to ensure accurate and thorough completion.
- Enter the date: Write the date of the entry at the top of the form.
- Fill in patient identification: Provide the patient's name (last, first, middle), grade, rank, rate, and the name of the hospital or medical facility.
- Input the register number: Enter the patient’s register number in the designated space.
- Specify the ward number: Write the ward number where the patient is located.
- Document progress notes: In the provided space, record the relevant observations, treatments, and any changes in the patient's condition.
After completing the form, it should be reviewed for accuracy and clarity before being filed in the patient's medical record. This ensures that all healthcare providers have access to the most current information regarding the patient's care.