Fill Your Tb Test Form
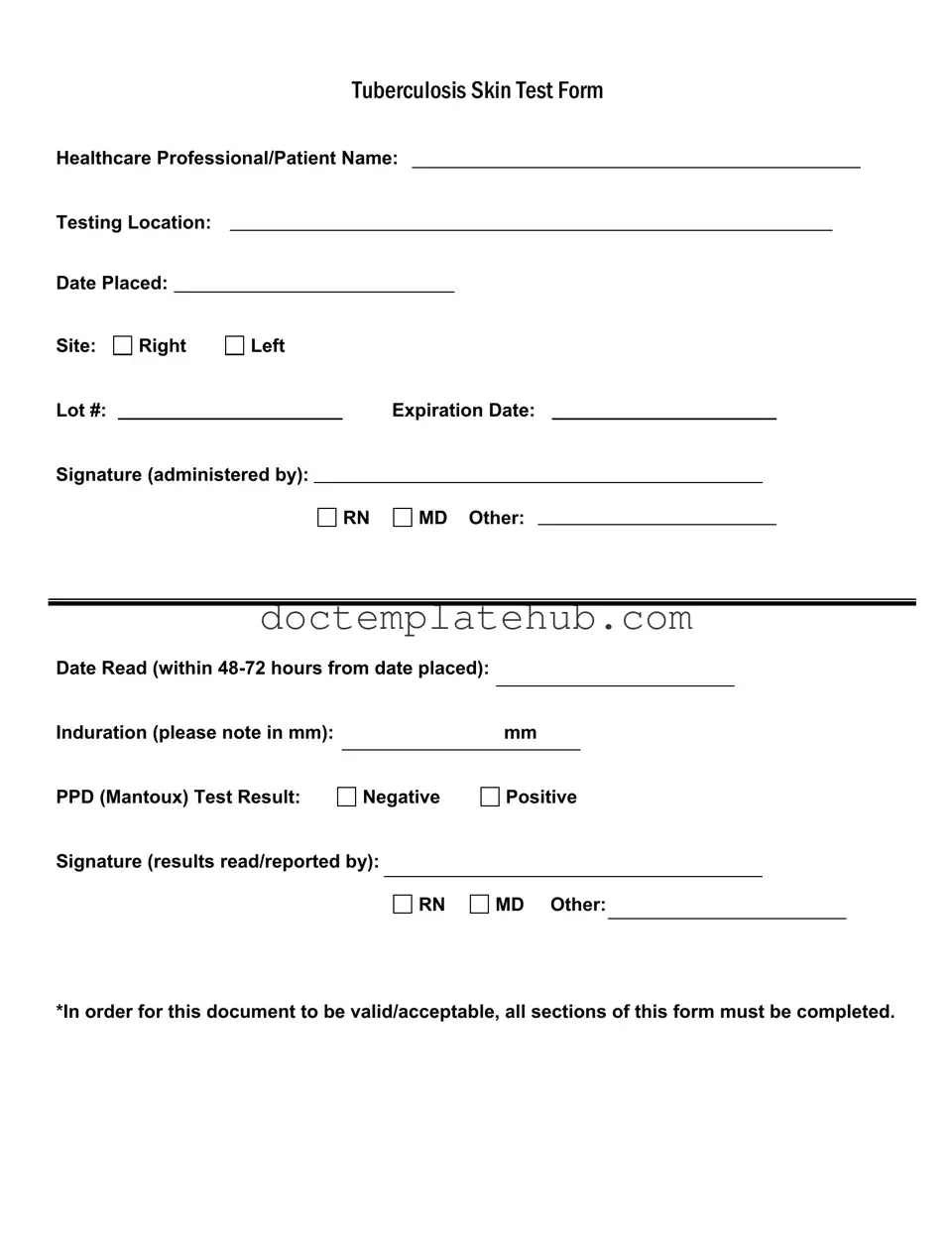
The Tuberculosis Skin Test form is a critical document used in healthcare settings to track and record essential information regarding TB testing. It captures the names of both the healthcare professional and the patient, ensuring clear identification. The form specifies the testing location and includes vital dates, such as when the test was placed and when the results were read, which must occur within 48 to 72 hours. The site of the test is noted, allowing for accurate monitoring of the test area. Additionally, the form requires details like the lot number and expiration date of the test material, which are crucial for maintaining compliance with health regulations. Induration measurements, recorded in millimeters, provide a clear indication of the test result, while the PPD (Mantoux) test result is marked as either negative or positive. Finally, signatures from the administering healthcare professional and the individual who reads the results are mandatory, confirming the accuracy and validity of the information provided. All sections of this form must be completed for it to be deemed acceptable, underscoring the importance of thorough documentation in public health efforts.
Similar forms
The TB Test form shares similarities with the Vaccination Record form. Both documents serve as official records of medical tests or vaccinations administered to an individual. They require details such as the patient’s name, the healthcare professional’s signature, and specific dates related to the administration and reading of the results. Just like the TB Test form, the Vaccination Record must be filled out completely to be considered valid, ensuring that all necessary information is documented for future reference.
Another document that resembles the TB Test form is the Medical Clearance form. This form is often used in various settings, including schools and workplaces, to confirm that an individual is free from contagious diseases. Similar to the TB Test form, it includes information about the individual, the healthcare provider, and the results of any relevant tests. Both documents emphasize the importance of thorough completion to ensure they are accepted by the institutions requiring them.
The Health Assessment form is also akin to the TB Test form. This document gathers comprehensive health information from patients, including past medical history, current medications, and test results. Like the TB Test form, it requires signatures from healthcare professionals and must be filled out entirely to be valid. Both forms aim to provide a clear picture of an individual’s health status, facilitating informed medical decisions.
The Employment Health Screening form is another similar document. It is commonly used by employers to assess the health of potential hires. This form often includes results from various health tests, including TB tests. Both forms necessitate the completion of specific sections and signatures from healthcare providers to ensure accuracy and validity. They serve the purpose of safeguarding public health by ensuring that employees are not carrying communicable diseases.
For those looking to understand property transfers better, the process often involves a Quitclaim Deed that serves as a straightforward means of conveying ownership without title guarantees. To learn more about this essential document, check out this resource on completing a Quitclaim Deed form.
The School Health Form bears resemblance to the TB Test form as well. Schools often require this document to ensure that students are up-to-date with vaccinations and screenings. Both forms collect similar information, including the student's name, the healthcare provider’s details, and test results. They must be filled out completely to be accepted by educational institutions, highlighting the importance of maintaining a healthy school environment.
The Travel Health Certificate is another document that shares similarities with the TB Test form. Travelers may need this certificate to confirm they have received necessary vaccinations or screenings before visiting certain countries. Like the TB Test form, it requires detailed information about the individual and the administering healthcare professional. Both documents must be fully completed to be considered valid for travel purposes.
Lastly, the Consent for Medical Treatment form is comparable to the TB Test form. This document is used to obtain permission from patients before administering tests or treatments. It includes patient information, details of the procedure, and signatures from both the patient and the healthcare provider. Like the TB Test form, it emphasizes the need for thorough completion to ensure all parties are informed and in agreement regarding the medical actions being taken.
Other PDF Templates
Affidavit of Support - Completing the I-864 involves providing personal income and household information.
Tattoo Artist Independent Contractor Agreement - The agreement contains all necessary components for legal compliance in the designated state.
When considering a Power of Attorney form in Texas, it's essential to seek resources that clarify the process and its important aspects; for instance, you can find useful templates and guidance at smarttemplates.net, which can aid in ensuring that your legal and financial matters are appropriately managed.
Crest of Arms - The design reflects values such as loyalty, valor, and honor.
More About Tb Test
What is the purpose of the TB Test form?
The TB Test form is designed to document the administration and results of the Tuberculosis skin test, commonly known as the PPD or Mantoux test. This form captures essential information such as the healthcare professional's name, the testing location, and the date the test was placed and read. It serves as an official record for both healthcare providers and patients, ensuring that all necessary details are noted for future reference.
What information needs to be filled out on the TB Test form?
To ensure the form is valid and acceptable, all sections must be completed. This includes the names of the healthcare professional and patient, the testing location, the date the test was placed, and the site of the injection (right or left arm). Additionally, the lot number and expiration date of the PPD solution must be recorded. The form also requires signatures from the administering professional and the individual who reads and reports the results, along with the induration measurement in millimeters and the test result (negative or positive).
How long after the test is placed should it be read?
The TB Test must be read within 48 to 72 hours after it has been placed. This time frame is crucial because it allows for accurate measurement of induration, which indicates the body's response to the test. Reading the test outside this window may lead to inaccurate results, necessitating a repeat of the test.
What does the induration measurement indicate?
Induration refers to the raised, hardened area at the injection site and is measured in millimeters. The size of the induration is critical for interpreting the test results. A positive result typically indicates that the individual has been exposed to the TB bacteria, while a negative result suggests no exposure. However, the interpretation may vary based on individual risk factors, such as recent exposure to TB, prior TB infection, or immunocompromised status.
Who is qualified to administer and read the TB Test?
The TB Test can be administered by qualified healthcare professionals, including registered nurses (RNs) and medical doctors (MDs). These professionals are trained to ensure the test is placed correctly and can accurately read and report the results. The signatures of the administering and reporting professionals on the form provide validation of the test process and results.
Dos and Don'ts
When filling out the TB Test form, it’s important to ensure accuracy and completeness. Here are some guidelines to help you navigate the process effectively.
- Do fill in all required sections of the form to ensure it is valid.
- Do double-check the dates, especially the date placed and the date read.
- Do use clear and legible handwriting to avoid any misunderstandings.
- Do confirm the testing location is accurately noted on the form.
- Don't leave any sections blank; incomplete forms can lead to delays.
- Don't forget to note the induration measurement in millimeters accurately.
- Don't use abbreviations or shorthand that may confuse the reader.
- Don't forget to sign the form where required, as this is essential for validation.
Tb Test - Usage Steps
After gathering the necessary information, you are ready to fill out the TB Test form. Ensure that all sections are completed accurately, as incomplete forms may not be accepted.
- Start with the section labeled Healthcare Professional/Patient Name. Write the name of the patient or the healthcare professional administering the test.
- Next, fill in the Testing Location. Provide the name of the facility where the test is being conducted.
- In the Date Placed field, enter the date when the test is administered.
- Indicate the Site of the test by marking either Right or Left.
- Record the Lot # of the test. This information can usually be found on the test kit packaging.
- Write down the Expiration Date of the test kit.
- In the Signature (administered by) section, sign the form. Indicate whether you are an RN, MD, or Other.
- Leave space for the Date Read. This should be filled in within 48-72 hours after the test is placed.
- Measure the Induration in millimeters (mm) and write this value in the designated space.
- Mark the PPD (Mantoux) Test Result as either Negative or Positive.
- Finally, in the Signature (results read/reported by) section, sign the form again and indicate your title (RN, MD, or Other).